Trans women ARE at risk for prostate cancer, whether or not they've had bottom surgery.
I was surprised to hear this information from a reader, and I suspect it may not be common knowledge, so I wanted to share what I've learned with you.
Early detection and treatment of prostate cancer can save a life, so this feels extremely important to know about!
(I am not a doctor or medical professional, and this article is merely a starting point for awareness, definitely not medical advice. Please consult your own medical professional and do your own research.)
Who is at risk of prostate cancer?
Around one in eight people with prostates will be diagnosed with prostate cancer in their lifetime, according to the American Cancer Society.
Trans women undergoing medical and surgical gender-affirming interventions have a 2 to 5 times lower risk of prostate cancer.
But many trans women are not interested in or do not have access to gender-affirming hormones or surgery. And regardless of your medical history, it feels important to know prostate cancer is a fairly common risk.
Any cancer diagnosis can be intensely scary, but most people diagnosed with prostate cancer do not die from it, especially with access to monitoring and treatment.
Prostate cancer tends to affect folks over 50 years old. If you medically transition in your 20’s or 30’s, even the most well-informed doctor is likely not going to think to mention prostate cancer.
A lot of health info about trans people is focused on younger adults. But you can be trans at any age, and older trans people deserve well-informed, inclusive medical care.
Prostate cancer in trans women
Prostate Cancer UK has an excellent, inclusive overview of prostate cancer in trans women:
Anyone with a prostate can develop prostate cancer. Let's consider who has a prostate.
Gender-affirming bottom surgery for trans women doesn't usually involve removing the prostate, as described by Harvard Health. The prostate is right next to the urethra. The urethra has the very important job of allowing us to pee, and it's not recommended to mess with a healthy prostate because it might affect the urethra as well. So leaving the prostate where it is leads to a safer bottom surgery with fewer side effects.
The prostate develops during puberty, with the higher amount of testosterone in the body. Anyone who went through a testosterone puberty has some amount of prostate. The reason I phrase it that way is because a study found that trans men on gender affirming hormone therapy develop prostate cells! (They took samples with consent from these folks during bottom surgery.) Trans men are not at risk of prostate cancer however that we know of.
Inclusive preventative care
Prostate cancer is both relatively common and relatively treatable if detected early. Being able to access preventative care is crucial.
For trans people, gender-inclusive healthcare providers make a huge difference in our ability to receive preventative care.
For my preventative healthcare, I should receive pap smears to check for cervical cancer and mammograms to check for breast cancer. These are commonly referred to as “well woman” care and similar, but, I feel so much more comfortable with a provider who just calls it a pap smear, for example, and asks me if I'm okay with doing this exam.
A prostate exam, similarly, should not be a gendered healthcare experience, as we know people of various genders may have a prostate.
Ideally, our healthcare providers would not refer to these exams in gendered ways, and our insurance would cover the body parts we actually have, and the receptionists would not be confused when a man tries to book a pap smear or a woman tries to schedule a prostate exam.
But, I want to acknowledge and empathize that most trans people unfortunately get misgendered as a cost of this preventative care. I appreciate that you are taking care of yourself in this way!
Black folks are at higher risk
Black people have an increased risk of prostate cancer. One in five Black men compared with one in nine men from the general population were diagnosed with prostate cancer.
While it is even more unlikely for Black trans women to receive respectful preventive health care due to racism in medical care, these statistics show how important this care is to save lives.
Healthcare providers need to step up and provide inclusive, preventative care to Black trans women.
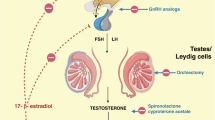
Hormones and prostate cancer
Hormones affect the growth of prostate cancer, but in a fascinatingly complicated way. Lower testosterone can potentially reduce your chances of developing prostate cancer, but reducing testosterone is not a good treatment for aggressive cases. This article from Duke Health explains that testosterone can actually be used as a treatment for advanced cases.
Similarly, estrogen can potentially have both helpful and detrimental effects towards prostate cancer. Some of this is because of the interaction with testosterone; people with estrogen-dominant hormones often are suppressing or not producing much testosterone.
Estrogen or hormone suppressing medications can be used to reduce testosterone levels for cancer treatment.
It seems to me that research to support the healthcare of trans people, if done ethically and respectfully, has the potential to better explain the effects of hormone therapy on cancer, with a population of people who thrive on gender-affirming hormone therapy.
This research would not only help trans people, it would help cis people as well, many of whom also use hormone replacement therapy or would consider it for a cancer treatment.
Exams and treatments for prostate cancer
So what kind of exams and treatments are available for people with prostates with access to quality healthcare?
The good news is that exams don't need to be as invasive as they used to be and treatments and active surveillance are often effective.
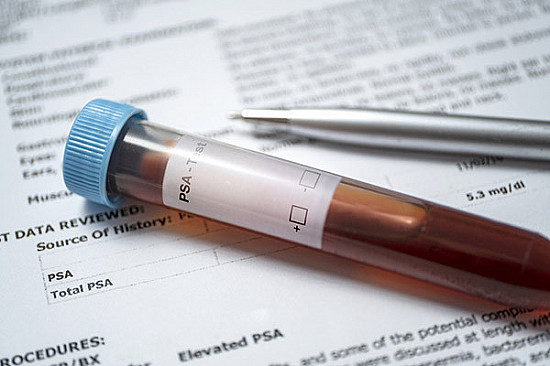
A prostate-specific antigen (PSA) blood test is often the first method of screening for problems with the prostate. PSA is a protein made by the prostate and a high level can indicate cancer or other issues.
But being on estrogen hormone therapy reduces the level of PSA, meaning the threshold for further screening likely needs to be lower than the threshold for cis men, for some trans women.

A PSA test is often how people are alerted to the possibility of prostate cancer (although not the only way, it is possible for a doctor to notice signs during a colonoscopy, for example).
If you have the BRCA gene, associated with breast cancer, be aware this gene can also be associated with prostate cancer. (And if you have developed breasts, consider breast cancer screenings as well!)
The next steps to check if someone has prostate cancer often include a digital rectal exam.
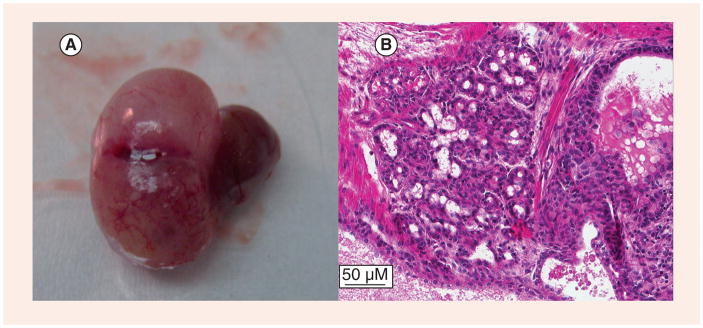
An official diagnosis of prostate cancer requires a biopsy, which can also indicate how likely the cancer is to grow and spread.
This article from the American Cancer Society describes the exams for diagnosis. Most of the article uses gender neutral language, actually, but there is a middle section that's like "men this," "men that," as if it's written by a different person.
After a diagnosis, treatments can include active surveillance, hormone injections, radiation, medications, and surgery.
Access to quality healthcare makes a huge difference in treatment. Just one more reason why respectful, inclusive, knowledgeable health care providers are so crucial.
It can still be really scary to find out you have this condition, but knowing and taking care is safer than not knowing.
To my readers who are living with prostate cancer, I send you my very best wishes for treatment and recovery.
And to my readers who know someone who might develop prostate cancer, consider sending them this article. Let's get the word out about preventative healthcare for all genders.
How has your experience been accessing preventative health care? Please let us know in the comments!
Are you trans and in the US? Take the Trans Health Survey from Point of Pride now to help build a better, more affirming future for trans healthcare:
Point of Pride provides trans people with access to life-changing, gender-affirming health and wellness services.
This survey is about centering trans people in conversations about our healthcare.
We're calling on trans people age 18+ across the United States to share their stories of care, challenges, and visions for a better future. Your responses are completely confidential and will help drive real change in how care is delivered and experienced.
Created by a team of trans advocates, researchers, and organizers, this national project centers safety, access, joy, and autonomy—because trans healthcare should be shaped by those who live it.
Take care,
Rey